Pulse Analytics is a multi-product web application that helps pharmaceutical clients identify and overcome barriers that prevent patients from receiving life-saving care.
At Pulse, I partner with our consulting branch, The Dedham Group, to translate complex healthcare concepts into intuitive data analytics tools.
A subset of the tools I’ve worked on are featured below. Due to my confidentiality agreement, I am only able to share high-level mockups of the application.
ux research
product design
ux/ui design
product management
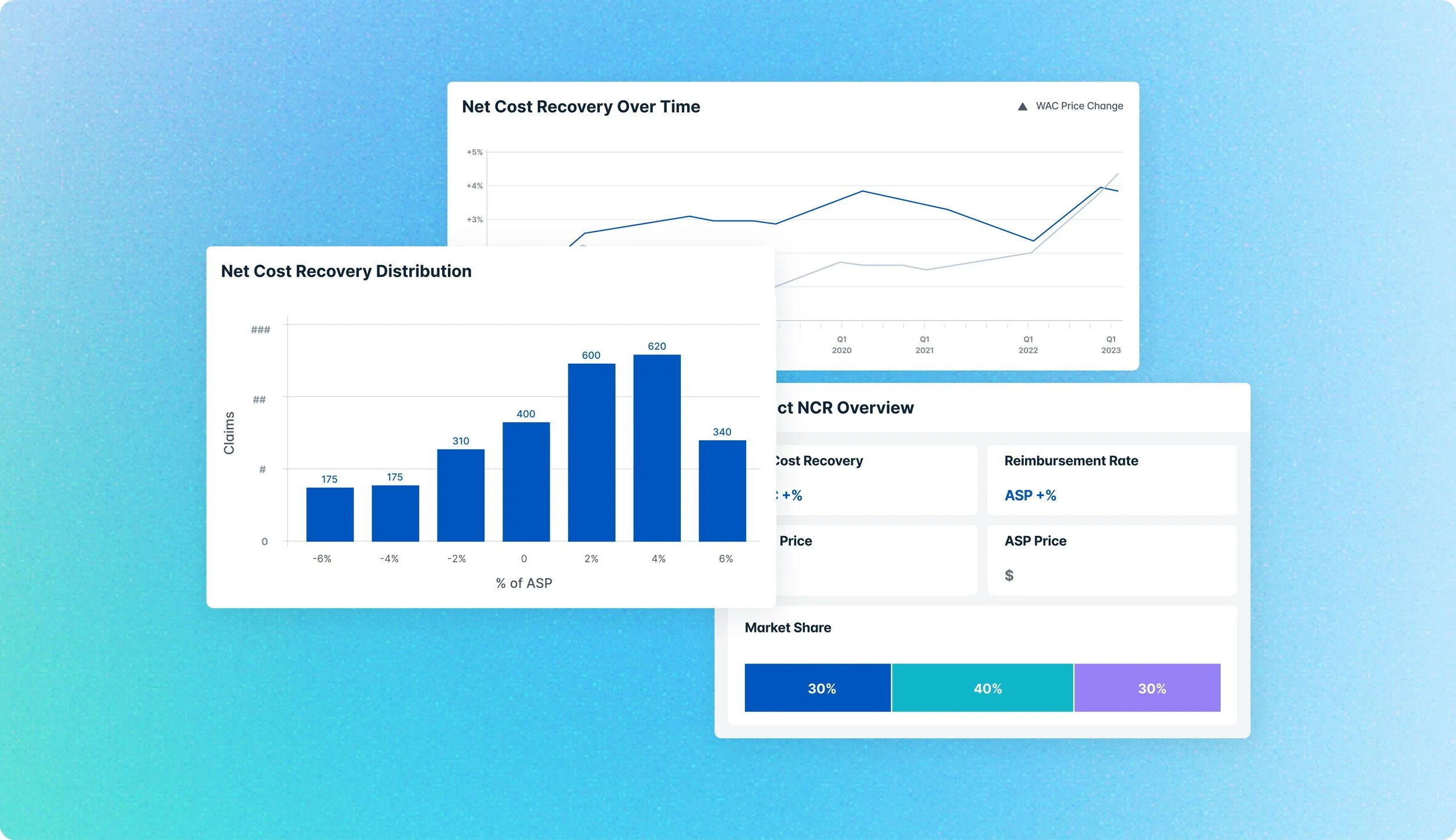
NET COST RECOVERY TOOL
The Net Cost Recovery Tool analyzes provider channel economics using medical claims data. The tool helps users understand reimbursement trends, net cost recovery dynamics, and their influence on account behavior to support more informed channel strategy decisions.
Conducted competitive research to evaluate the market landscape and identify opportunities for differentiation
Analyzed the strengths and limitations of claims data to guide feature prioritization
Defined the product’s structure and information architecture to support user goals
Designed new design system components to support tool features, including a date-range picker and settings toggle
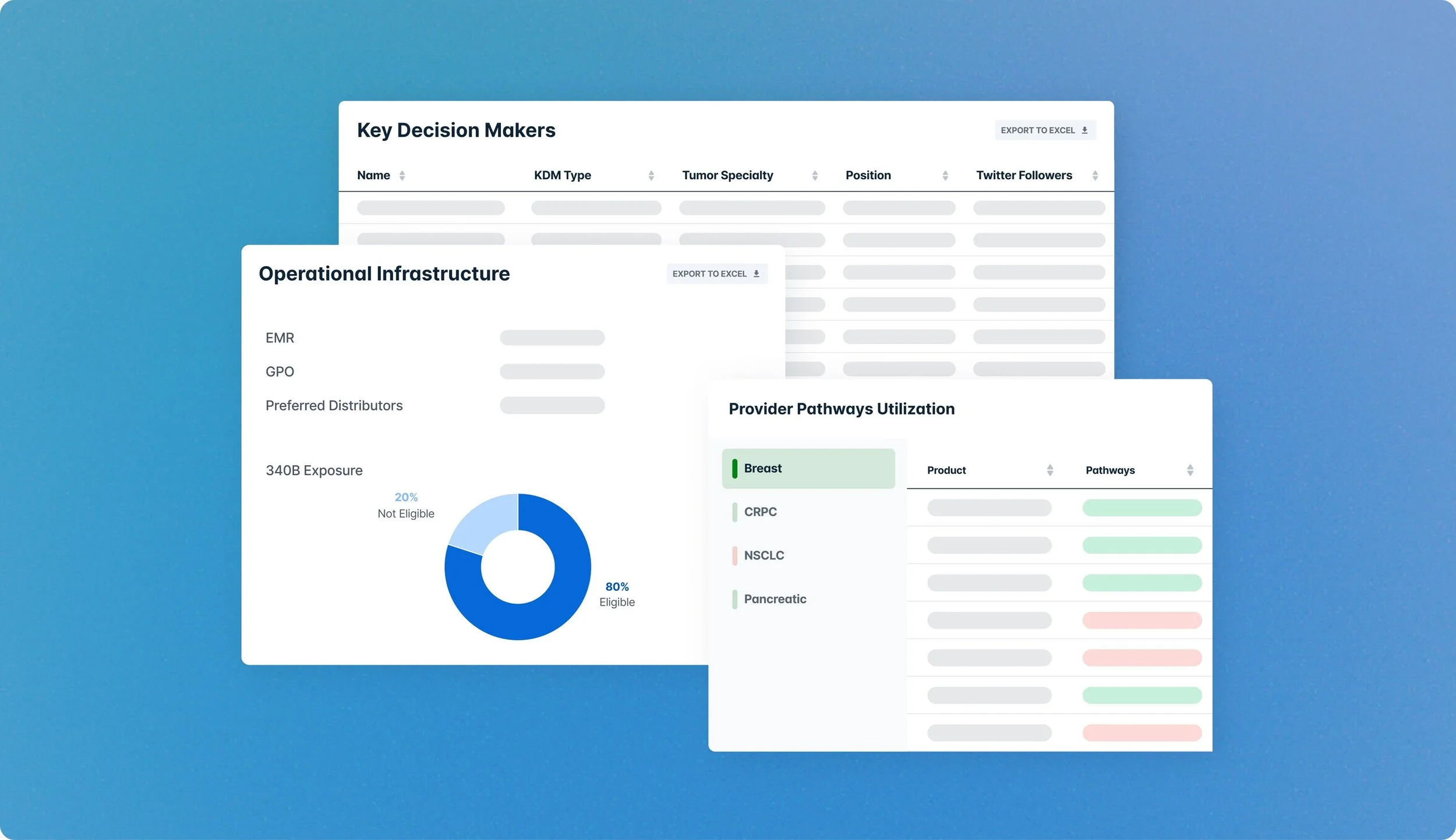
ONCOLOGY PROVIDER TOOL
The Oncology Provider Tool enables clients to better understand high-impact provider accounts by analyzing indication-specific clinical, operational, and economic behaviors and trends at hospitals and care centers across the US. Client research projects often generate large, complex data sets that are translated into custom feature add-ons to the Provider Tool.
Collaborated with consultants to understand the goals and key findings of each research project, then translated those insights into intuitive, client-facing features that highlight the most important and actionable data trends
Ensured the final designs are clear and aligned with the client's strategic needs
Conducted user surveys to learn NPS score and identify areas for improvement
PAYER QUALITY OF ACCESS TOOL
The Payer Quality of Access tool helps clients evaluate insurance coverage for their products, highlighting which restrictions are most burdensome to patients and how their product coverage compares to competitors. Clients can evaluate access at a regional-, state- or payer-level, informing targeted account engagement strategies to secure favorable payer access.
Audited user analytics, synthesize client feedback and conduct competitive research to identify existing pain points and areas for potential feature expansion
Utilized the ICE prioritization method to evaluate features and create product roadmap
Modernized outdated and difficult-to-navigate pages
Designed & implemented Pendo guides for new feature releases